I’m still astonished every time we do it. I mix my son’s clotting factor three times per week, before breakfast, then I infuse lifesaving medicine into one of his tiny little boy veins. I never imagined – in a million years – that I would do this. But, then I met my son. My son has hemophilia. Many people have asked me if I knew he had hemophilia when I adopted him. (That question still takes me by surprise.) Did I know? Yes. The precious boy who I knew was my son just happened to have hemophilia. We have learned together how to treat his condition, which is very manageable in the United States where we live. His day-to-day life looks pretty much like that of any other boy, aside from brief infusion treatments before breakfast three days per week. He goes to public school, participates in recess (including climbing high on the jungle gym!), participates in all activities in physical education, and is incredibly active in his free time, running, jumping, and having lots of fun. Treating his hemophilia is just a tiny part of his very busy, normal life.
Basics of Hemophilia and Its Treatment
To understand how to treat hemophilia, it’s helpful to know alittle bit about the condition. Hemophilia is an inherited bleeding disorder in which a person’s body does not make enough of one of the proteins needed for blood to clot properly. Hemophilia can be moderate (with 6-50% the normal level of clotting factor), mild (with 1-5% of the normal level of clotting factor), or severe (with less than 1% of the normal level of clotting factor). My son has the most common type of hemophilia, Hemophilia
A, which means that his body does not make Factor VIII (Factor 8); and, his hemophilia is severe. Put simply, my son’s missing factor means that his blood doesn’t have all the pieces it needs to form an effective clot.
There are 13 proteins, or blood clotting factors, that stack up –one after the other – to form a strong clot in a typical person’s blood. You can think of this process as much like lining up a series of dominoes when we were kids (or maybe even adults) to watch them all fall in succession. The problem with hemophilia is that one of those dominoes is missing. You can imagine what would happen if we took a domino out of a neatly arranged row before pushing the first domino down. They would stop falling once they got to the missing piece. Similarly, when my son’s body tries to form a clot, whether it’s external because of a skinned knee or internal because of a twisted ankle, his blood clotting factors stop stacking up at Factor 7, rather than proceeding to Factor 13 as in a typical person’s blood clotting process.
You may wonder how we fix this problem. The standard treatment for hemophilia is to replace the missing clotting factor by injecting it into the bloodstream so that it’s there, ready to make the blood clotting process proceed smoothly, when needed. The replacement Factor VIII doesn’t last very long in the bloodstream, though. So, in severe hemophilia we must replace it on a regular basis to prevent bleeding. This is called prophylactic treatment or prophylaxis (prophy for short).
What Does Treatment Look Like?
What does treatment look like at my house? We have a plastic tray that we call the “factor tray” where we arrange supplies and factor for each infusion. We keep that in a kitchen cabinet until infusion time. And, we have one kitchen cabinet, called the “factor cabinet” where we store all of our infusion supplies. In addition to shipping the clotting factor to our home, our home health company provides all the supplies we need to do infusions: tourniquets, butterfly needles, pre-filled saline syringes, empty syringes to hold the factor, gauze pads, alcohol wipes, and bandages (including my son’s favorite character bandages, upon request). They also provide reusable, gel packs that can be warmed to heat the infusion site to ensure my son’s veins are ready to receive factor. (All families get these supplies, whether they are infusing on their own or whether a home health nurse comes to do the infusions.) Before I wake my son on a “factor day” – Sunday, Tuesday, and Thursday for us – I mix his factor and set up the infusion supplies on the tray. This involves opening sterile gauze pads and a bandage, making sure we have alcohol wipes on the tray, and filling the tubing attached to the butterfly needle with sterile saline. We do this just in case we need to change the needle so that we don’t lose any factor in the tubing. I also heat a pot of water that I use to warm the gel pack for heating the infusion site.

Then, I wake my son, put warm sweatpants and a long-sleeved shirt on him, and we snuggle under blankets and read books or watch videos for about 15 to 20 minutes while he drinks orange juice. These activities ensure that his veins are ready to receive factor: the orange juice ensures that he is hydrated, and the warm clothes and blankets ensure that his veins are warm and expanded. Our goal is for him to have “fluffy veins” because they are much easier to find! See this link on the Hemophilia Federation of America’s website for more tips and tricks for smoother infusions. When we were first transitioning to Mommy-administered infusions, we read ALL of Laurie Kelley’s wonderful toddler books about hemophilia before EVERY infusion. They helped my son prepare mentally and emotionally, and they also helped my son develop essential knowledge about his condition so that he better understood reasons for and the process of infusions. These books are available free to all families at the link above.
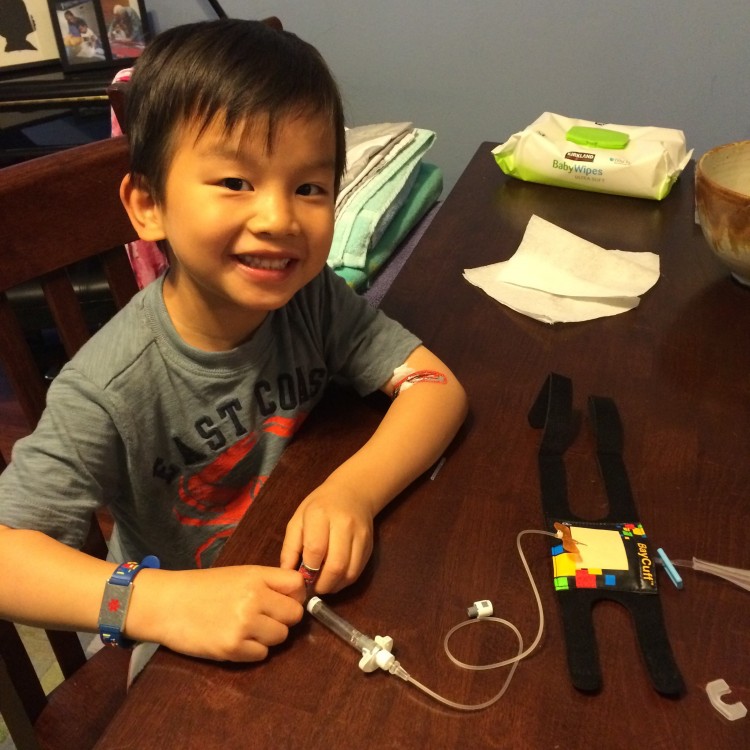
We infuse at the kitchen table. My son chooses a video on the iPad, and he eats Starburst candy during the infusion process. (Yes, my son eats candy before breakfast – but I’m ok with it because it gets him through the infusion!) I alternate arms so that his veins get a break between infusions. Before beginning, I warm the area to be infused with a heated gel pack. Then, I put the tourniquet around his arm, on top of his shirt, above his elbow. I feel the vein to make sure it’s springy and to locate its angle under the skin. Then, I wipe the infusion site  with alcohol. When it’s time for “the stick,” I focus on the vein and its angle under the skin. Inserting the needle into the vein (also called accessing the vein) is like landing an airplane on a runway – you don’t need to hold the needle at much of an angle to guide it into the vein. We use 27 gauge needles, the smallest available, because they leave less scar tissue (see the gray needles in the picture). Once theneedle is in the vein, I slowly push the factor (usually 2 to 4 ml of liquid) into the vein, while continuing to hold the needle. Then, I crimp the end of the tubing on the butterfly needle and switch the factor syringe for the saline syringe, so that I can use the saline to flush every last bit of factor out of the tubing and into my boy! (Our HTC nurse says every unit of factor counts!) After all the factor has been infused, I remove the needle and hold pressure on the infusion site with gauze and my thumb for about a minute. I fold the gauze pad so that it’s thick enough to continue compressing the infusion site when it’s secured under a bandage. Then, we’re all done! The whole infusion process takes about 10 minutes or less. Sometimes my son wants to push the factor, hold the needle, or pull the needle out, and I let him participate as much or as little as he wants. He has successfully accessed my vein with just one stick and tells me that he will infuse himself when he is 8. I don’t doubt that he will!
with alcohol. When it’s time for “the stick,” I focus on the vein and its angle under the skin. Inserting the needle into the vein (also called accessing the vein) is like landing an airplane on a runway – you don’t need to hold the needle at much of an angle to guide it into the vein. We use 27 gauge needles, the smallest available, because they leave less scar tissue (see the gray needles in the picture). Once theneedle is in the vein, I slowly push the factor (usually 2 to 4 ml of liquid) into the vein, while continuing to hold the needle. Then, I crimp the end of the tubing on the butterfly needle and switch the factor syringe for the saline syringe, so that I can use the saline to flush every last bit of factor out of the tubing and into my boy! (Our HTC nurse says every unit of factor counts!) After all the factor has been infused, I remove the needle and hold pressure on the infusion site with gauze and my thumb for about a minute. I fold the gauze pad so that it’s thick enough to continue compressing the infusion site when it’s secured under a bandage. Then, we’re all done! The whole infusion process takes about 10 minutes or less. Sometimes my son wants to push the factor, hold the needle, or pull the needle out, and I let him participate as much or as little as he wants. He has successfully accessed my vein with just one stick and tells me that he will infuse himself when he is 8. I don’t doubt that he will!
How Did We Get Here?
When my son first came home, our Hemophilia Treatment Center (see list of Hemophilia Treatment Centers here) and home health company set us up with a wonderful pediatric infusion nurse who was very familiar with hemophilia treatment, having treated another young boy for about seven years. And, she was GIFTED. She knew how to put my son at ease and had infinite patience. She also worked to help him feel control over his infusion process, giving him age-appropriate jobs to do, knowing that his early infusion experiences build skills and attitudes that he will carry with him for the rest of his life. She also helped us establish a routine that laid the foundation for the things we do now. That routine even included a small stuffed bear that my son would infuse before his own infusion began! Eventually we switched to his stuffed shark, and now he doesn’t even need to infuse a friend before we infuse him. I can’t say enough about making sure you have a good home health nurse. Insist on good care and keep trying until you find a person or routine that works for your child. When our lovely nurse was planning to move out of state, and my son desired to travel to other states (taking us away from our infusion nurse), that provided the impetus for me to learn – and for my son to be eager for me to learn! I practiced with a BayCuff kit, provided by a kind pharmaceutical representative. Then, I practiced on willing adults until I was confident in my ability to access veins. And, finally, one day when our nurse could not get to our house because of icy roads, I infused my son. When we were finished, he kissed me and said, “Mommy, thank you for doing factor!” Was it difficult to stick my son? You bet! My knees shook the whole time, and they continued to do that for weeks (maybe months). I didn’t want to hurt him, and I didn’t want to make a mistake. I know, though, that the pain of untreated bleeds is far greater than the tiny pain of a little needle stick. Now that I have been infusing him for almost two years, my son trusts me to do it. He doesn’t even flinch. My knees don’t shake. My son understands why he needs factor, and the whole process has become routine.
If you are considering adopting a child with this need, know that you can do this. I am NOT a nurse. I’m just a regular parent who learned to do what was needed to take care of my son. The tight knit hemophilia community also provides wonderful support and encouragement. Don’t let hemophilia treatment scare you. If I and my 6-year-old can access veins, you can, too!
These 4 boys with hemophilia wait on RainbowKids for their forever families. Click on Neil, Evan, Adrian and Mayson's name to learn more about each remarkable child.
